Briefing Note – Bowel Cancer
Briefing Note on Bowel Cancer in the UK
Bowel cancer is one of the most common cancer types. Sometimes it is referred to as colorectal cancer, which is another name for the disease. Bowel cancer in general has been rising in the past few decades and there are many theories for this rise. Please read below for the latest developments in bowel cancer and also tips on how to prevent it.
Background
Bowel cancer accounts for 11% of all new cancer cases in the UK. Every year, about 42,300 people are diagnosed with bowel cancer in the UK. 1 in 15 men and 1 in 18 women will get bowel cancer during their lifetime. Many risk factors influence your bowel cancer risk: age, obesity, and diet are the main risks.
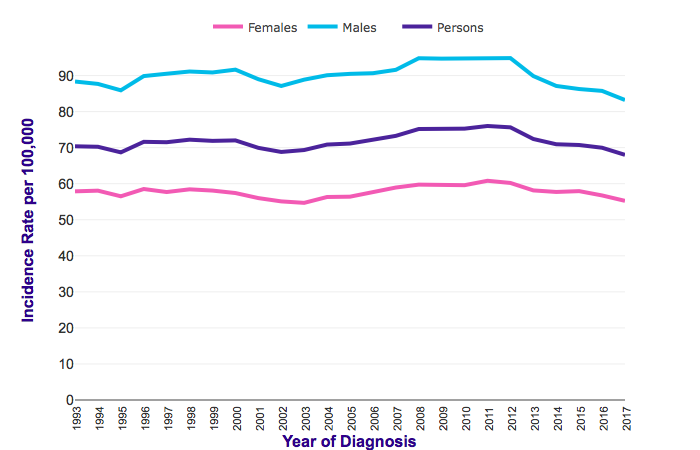
However, shorter term, the overall trend for bowel cancer in the UK is decreasing. Although bowel cancer cases were rising between 1971 and 1998, there was then a period of no new increases until 2012. Since 2012, we seem to be getting on top of the disease. The rate of new cases decreased by 4% in the last decade. However, still around 70 in 100,000 people are diagnosed with bowel cancer in the UK every year.
What are the risk factors?
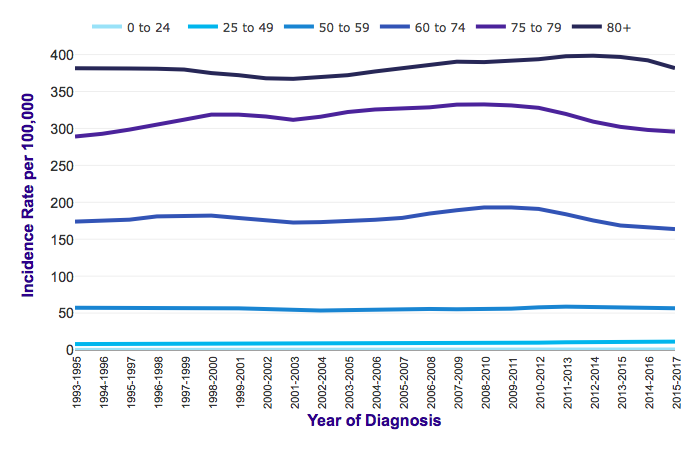
The main risk factor is age: your risk of getting bowel cancer increases dramatically with your age. The majority of people with bowel cancer are typically above 80 years old and the rest above 50. The rate of new cases in people aged below 50 years old is extremely low (Cancer Research UK, 2015-2017). The average age at the time of diagnosis is between 63-72 for colon and rectal cancers.
This may be due to your lifestyle that affects your risk during your lifetime. There are many risk factors that are well-known to increase risk of bowel cancer:
- Diet especially lack of dietary fibre and over consumption of red meat
- Obesity and being overweight
- Smoking
- Alcohol
- Previous cancer history
- Medical conditions (IBS, colitis, chronic inflammation)
- Radiation
- Infections
- Hereditary conditions
Some reports in the media may also mislead you into thinking that mobile phones, artificial sweeteners, genetically modified foods or plastic bottles are risks. However, not all these ‘facts’ are true. Many of them are not backed up by scientific studies. You can read more about the biggest myths around bowel cancer here:
https://www.cancerresearchuk.org/about-cancer/causes-of-cancer/cancer-myths
The key fact is that eating fibre reduces your risk of bowel cancer by at least 20%. 9 out of 10 people in the UK are not eating the recommended amount of fibre every day. Many scientific studies have linked the reduction in bowel cancer cases with dietary fibre. Interestingly, increased refrigerator use was linked to reduced gastric cancer risk in Asia –possibly also in Western countries. Similarly, antibiotics were linked to some types of bowel cancer, but were found to prevent others. Aspiring use, calcium and vitamin D are thought to prevent your risk of bowel cancer. Chronic inflammation and changes in your gut microbiome may also contribute to your bowel cancer risk. However, care is needed when interpreting bowel cancer risk factors from isolated studies. Scientific studies need to be repeated across continents to establish a relationship between a risk factor and cancer.
Bowel cancer in young adults
Worryingly, since 2010, the number of new cases among people aged 20-39 years old increased sharply by 5-19%. Since bowel cancer is significantly associated with lifestyle and diet, the main explanation would be the rising levels of obesity and diabetes in younger population. Moreover, young people nowadays tend to be less physically active and may have a higher consumption of red meat, increasing their bowel cancer risk.
Source: Cancer Research UK, https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer/incidence#heading-Two, Accessed 05/2020
Bowel cancer and sex
Bowel cancer is more common among men than women. Men form almost 56% of all cases, whereas women only 44%. This may be due to different lifestyle habits: women tend to be more interested in healthy diet, exercise and general healthy lifestyle than men, reducing their bowel cancer risk. Perhaps interestingly, women also tend to have a better prognosis than males. This was in past linked to differences in hormonal levels.
Source: Cancer Research UK, https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer/incidence#ref-2, Accessed 05/2020
Bowel cancer prevention
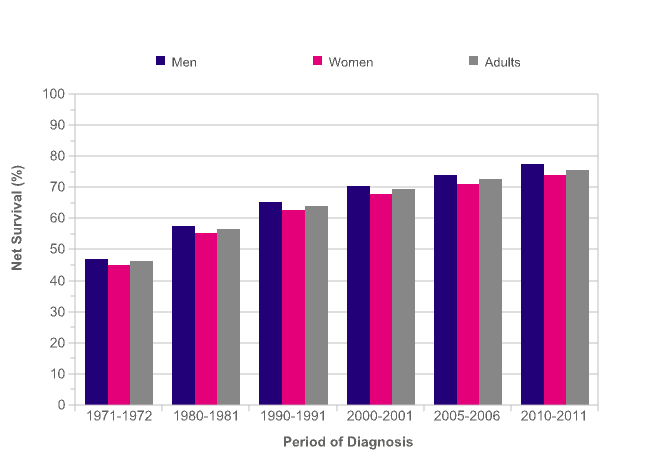
The main factor contributing to decreasing levels of bowel cancer is screening. The UK has a national screening programme for bowel cancer, that helps to reduce bowel cancer incidences and severity thanks to early diagnosis. In 2011, a ‘Be Clear on Bowel Cancer’ campaign was launched to promote bowel cancer awareness. This helped to improve the bowel cancer statistics drastically, possibly by removing the stigma around diagnostic procedures. If people feel that going for colonoscopy can be part of a yearly check-up and there is no shame associated with it – more people seek early diagnosis and treatment for bowel conditions, in turn helping to prevent bowel cancer. Probably thanks to improved screening and awareness, the survival for bowel cancer patients has been steadily improving by almost 60% since 1971.
Source: Cancer Research UK, https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer/survival#heading-Two,accessed 05/2020
Bowel Cancer in the UK
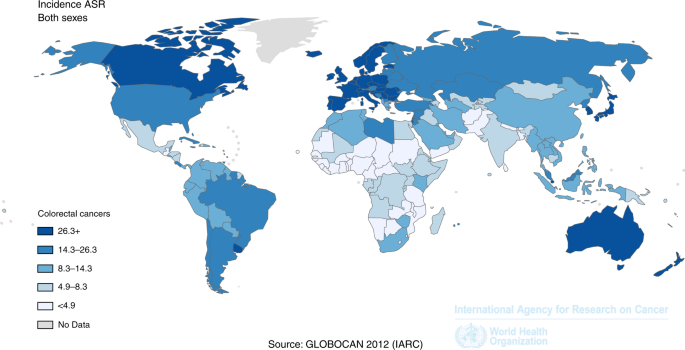
Despite the awareness campaign the age standardised incidence rate of bowel cancer in the UK is amongst the highest in the world. Many Western countries have high rates of bowel cancer among their population, including Germany, Spain, Canada and Australia. This may be due to low levels of dietary fibre, poor lifestyle, consumption of red meat, alcohol and smoking.
Lifestyle factors are likely to contribute to a poorer survival rate in the UK than in other countries. France, Canada and United States have higher survival rates for colorectal cancer than the UK. Although the UK has been improving its survival rate over the last decade with the screening programmes playing a significant role in catching bowel cancer in its earliest stages and improving patients’ prognosis. Awareness around bowel cancer and its risk factors is still low in the UK, in contrast to the US.
A main difference between the UK and US is also in clinical recommendations. UK NICE guidelines do not recommend endoscopy or imaging for people with irritable bowel syndrome (IBS). However, almost half of IBS patients in the US receive endoscopy, possibly detecting early-stage tumours more often. Colonoscopy is the primary screening method for early-stage colorectal cancers. Getting people at risk of bowel cancer to the doctor in the UK earlier will improve the risk and prognosis.
Source: The colorectal epidemic: challenges and opportunities for primary, secondary and tertiary prevention. (Brenner and Chan 2018)
The future and prevention of bowel cancer
Prevention and early detection play significant roles in reducing your risk of bowel cancer, and your prognosis if you are diagnosed. Eating a high fibre diet, avoiding tobacco and alcohol consumption, eating less red meat and improving your exercise habits will all help in reducing your risk of bowel cancer.
But the good news is that there are several trials underway to further reduce your risk, for example scientists are trialling low dose aspirin for preventing bowel cancer, as well as improvements to bowel cancer screening. We encourage you to join our campaigns against the incidence of bowel cancer as well as other life threatening cancers.
Taking care of your body and gut will not only improve your bowel cancer risk, but also lifestyle and quality of life.
Produced by the CancerWatch team, Summer 2020
References
Bowel cancer statistics [WWW Document], 2015. . Cancer Research UK. URL https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer (accessed 5.22.20).
Brenner, H., Chen, C., 2018. The colorectal cancer epidemic: challenges and opportunities for primary, secondary and tertiary prevention. British Journal of Cancer 119, 785–792. https://doi.org/10.1038/s41416-018-0264-x
Center, M.M., Jemal, A., Smith, R.A., Ward, E., 2009. Worldwide Variations in Colorectal Cancer. CA: A Cancer Journal for Clinicians 59, 366–378. https://doi.org/10.3322/caac.20038
Exarchakou, A., Donaldson, L.J., Girardi, F., Coleman, M.P., 2019. Colorectal cancer incidence among young adults in England: Trends by anatomical sub-site and deprivation. PLOS ONE 14, e0225547. https://doi.org/10.1371/journal.pone.0225547
Keum, N., Giovannucci, E., 2019. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nature Reviews Gastroenterology & Hepatology 16, 713–732. https://doi.org/10.1038/s41575-019-0189-8
Kunzmann, A.T., Coleman, H.G., Huang, W.-Y., Kitahara, C.M., Cantwell, M.M., Berndt, S.I., 2015. Dietary fiber intake and risk of colorectal cancer and incident and recurrent adenoma in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial12. Am J Clin Nutr 102, 881–890. https://doi.org/10.3945/ajcn.115.113282
Loomans-Kropp, H.A., Umar, A., 2019. Cancer prevention and screening: the next step in the era of precision medicine. npj Precision Oncology 3, 1–8. https://doi.org/10.1038/s41698-018-0075-9
Mármol, I., Sánchez-de-Diego, C., Pradilla Dieste, A., Cerrada, E., Rodriguez Yoldi, M.J., 2017. Colorectal Carcinoma: A General Overview and Future Perspectives in Colorectal Cancer. Int J Mol Sci 18. https://doi.org/10.3390/ijms18010197
Murphy, N., Norat, T., Ferrari, P., Jenab, M., Bueno-de-Mesquita, B., Skeie, G., Dahm, C.C., Overvad, K., Olsen, A., Tjønneland, A., Clavel-Chapelon, F., Boutron-Ruault, M.C., Racine, A., Kaaks, R., Teucher, B., Boeing, H., Bergmann, M.M., Trichopoulou, A., Trichopoulos, D., Lagiou, P., Palli, D., Pala, V., Panico, S., Tumino, R., Vineis, P., Siersema, P., van Duijnhoven, F., Peeters, P.H.M., Hjartaker, A., Engeset, D., González, C.A., Sánchez, M.-J., Dorronsoro, M., Navarro, C., Ardanaz, E., Quirós, J.R., Sonestedt, E., Ericson, U., Nilsson, L., Palmqvist, R., Khaw, K.-T., Wareham, N., Key, T.J., Crowe, F.L., Fedirko, V., Wark, P.A., Chuang, S.-C., Riboli, E., 2012. Dietary Fibre Intake and Risks of Cancers of the Colon and Rectum in the European Prospective Investigation into Cancer and Nutrition (EPIC). PLoS One 7. https://doi.org/10.1371/journal.pone.0039361
Soriano, L.C., Soriano-Gabarró, M., García Rodríguez, L.A., 2018. Trends in the contemporary incidence of colorectal cancer and patient characteristics in the United Kingdom: a population-based cohort study using The Health Improvement Network. BMC Cancer 18, 402. https://doi.org/10.1186/s12885-018-4265-1
Yan, S., Gan, Y., Song, X., Chen, Y., Liao, N., Chen, S., Lv, C., 2018. Association between refrigerator use and the risk of gastric cancer: A systematic review and meta-analysis of observational studies. PLoS One 13. https://doi.org/10.1371/journal.pone.0203120
Yang, Y., Wang, G., He, J., Ren, S., Wu, F., Zhang, J., Wang, F., 2017. Gender differences in colorectal cancer survival: A meta-analysis. International Journal of Cancer 141, 1942–1949. https://doi.org/10.1002/ijc.30827

